Paying For Social Care: Investing in What Matters
By Rae Anstett
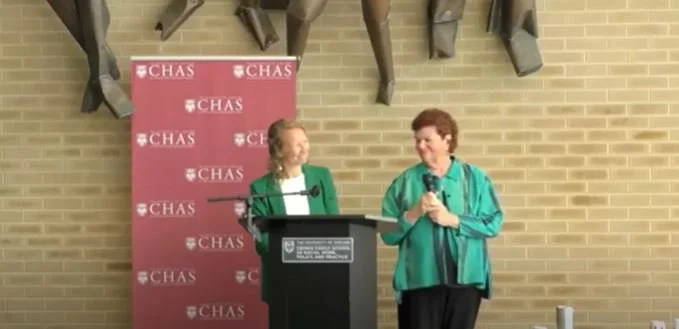
On September 26th, CHaSCI leaders Bonnie Ewald and Robyn Golden were invited by the Center for Health Administration Studies at the University of Chicago Crown Family School of Social Work to give a lecture entitled Paying for Social Care: Investing in What Matters as part of the Michael M. Davis Lecture Series.
In this lecture, our CHaSCI leaders addressed the hard-fought and ever-expanding imperative to invest in person-centered social care as a standard within the scope of the dominant medical system. This type of care improves the access, delivery, and outcomes of healthcare. As a barrier to the attainment of these equitable health outcomes though, they cited a lack of financial resources, which act as a means of direct institutional support for social care activities.
The following takeaways from the lecture outline how social care improves health equity but necessitates increased structural and financial investment:
Social determinants of health—or the conditions in which people are born, grow, and live— health behaviors, and the physical environment are estimated to impact 80% of health outcomes.
This impact stems from how psychosocial challenges displace patients’ focus and energy from taking care of medical conditions.
Social workers are experts in providing social care that supports people’s well-being across socioeconomic conditions.
While healthcare costs are high and systems are not delivering at scale, investment in social care is associated with reduced costs and positive health outcomes.
A variety of healthcare stakeholders—including individual providers, plans, and governmental sectors—must ask the question of how to invest in positive relationships between patients and providers.
(I.e., relationships that are first-name, caring, advisory, and friendly as opposed to those characterized by patients as harassing, overbearing, or clinical)
Grant, healthcare, and governmental funding sources are typical financial supports for social care, but gradually pushing the envelope on prevention to encompass social work requires expanding the Centers for Medicare & Medicaid Services (CMS) and coordination between funding sources.
The future of health equity depends on investment in social care.